Cobenfy breaks new ground as the initial antipsychotic medication designed to address schizophrenia through the modulation of cholinergic receptors rather than dopamine receptors.
The approval of Cobenfy by the U.S. Food and Drug Administration (FDA) on September 26 marked a milestone in the treatment of schizophrenia. This newly approved medication, a blend of xanomeline and trospium chloride, boasts a unique mechanism of action that distinguishes it from traditional medications known for their side effects. Despite introducing its own set of side effects, Cobenfy offers a promising alternative for individuals battling schizophrenia.
Schizophrenia stands out as a highly severe psychiatric condition, leading to significant repercussions such as social alienation, stigmatization, and reduced likelihood of forming relationships. Individuals affected by schizophrenia face a reduced lifespan of 13-15 years, attributed to factors like weight increase, unhealthy eating patterns, smoking, and concurrent substance abuse. An alarming five percent of individuals with schizophrenia succumb to suicide.
Approximately one out of every hundred individuals will experience schizophrenia during their lifetime. Recent research has cast doubt on the assumption that this condition affects both genders equally, revealing a slightly higher prevalence among men. This mental disorder typically emerges in late adolescence or early adulthood, with peak onset observed in males in their early 20s and in females in their mid- to late 40s.
Understanding the impact of Cobenfy’s innovation and its potential for change necessitates a deep grasp of the diverse repercussions of schizophrenia, its diagnosis, and the scientific community’s comprehension of its underlying causes.
Symptoms exhibited in clinical cases of schizophrenia
Prodromal symptoms are commonly observed in the majority of individuals who develop schizophrenia. These symptoms typically persist for approximately less than a year and can manifest as unexplained sensations of internal transformation, emergence of new spiritual and philosophical pursuits, feelings of anger, irritability, anxiety, sadness, and a tendency to isolate oneself socially.
In schizophrenia, the clinical presentation can be categorized into three main groups: reality distortion, disorganization, and negative symptoms. The positive symptoms include delusions, hallucinations, and a form of speech that is hard to comprehend, which is clinically known as formal thought disorder.
In 1911, the Swiss psychiatrist Paul E. Bleuler introduced the concept of schizophrenia using the “four As”: affect, associations, ambivalence, and autism. Over time, descriptions of the disorder have evolved to encompass a broader spectrum of symptoms, including negative aspects such as diminished speech output, decreased goal-oriented behavior, lack of interest or drive, decreased energy levels, diminished pleasure, and reduced emotional expression.
Ineptitude indications encompass formal thought disorder (also deemed a positive symptom), disarrayed conduct, and improper affect. A fascinating sign that has presently become less prevalent, notably in economically advanced nations, is catatonia: distinguished by an array of abnormal motor actions manifesting with stupor or agitation. It is no more exclusively linked with schizophrenia since it is also observed in other mental health conditions.
Kurt Schneider, a renowned German psychiatrist, identified specific symptoms known as “first rank” symptoms which were traditionally associated with schizophrenia. These symptoms encompassed auditory hallucinations where the patient hears voices talking about them in the third person, alterations in the sense of control over one’s thoughts, and the feeling of external influences governing one’s actions, physical sensations, and emotions.
Cognitive impairment is ubiquitous in schizophrenia. Patients have shown impaired performance on various cognitive tests that measure judgement, attention, memory, and general intellectual functions.
The origin of schizophrenia – what triggers it?
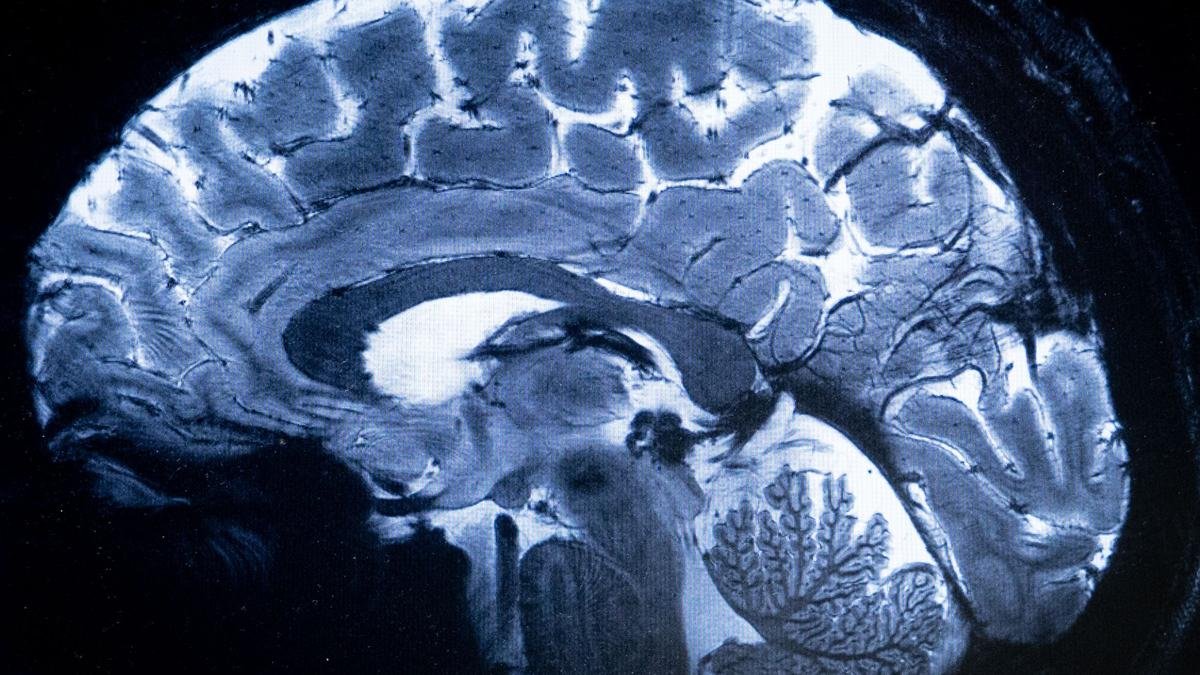
Schizophrenia, a complex disorder, cannot be understood through a singular perspective. The significance of genetics in the development of schizophrenia cannot be overstated. Specific genetic variations linked to risk directly impact the brain by altering gene expression, leading to disturbances in brain development and functionality.
In 2014, a comprehensive genetic study pinpointed 108 genetic loci linked to schizophrenia, emphasizing that correlation is not the same as causation. While conditions such as Huntington’s disease, cystic fibrosis, hemochromatosis, and sickle cell anemia stem from mutations in single genes, schizophrenia stands out as polygenic, involving hundreds, or even thousands, of genes with minor impacts. Additionally, rare genetic variations with significant effects have also been uncovered in relation to schizophrenia.
Neurodevelopmental theory posits that schizophrenia can stem from various factors such as experiences during infancy, at birth, or even in the womb. Prenatal and perinatal challenges stand out as the predominant environmental triggers for schizophrenia. The interplay between genetic predispositions for schizophrenia and early-life adversities escalates the likelihood of developing the disorder by up to five times in the presence of such complications.
Our comprehension of the pathophysiology of schizophrenia has been enriched by the identification of genes linked to increased risk and the exploration of the neurodevelopmental roots of the disorder.
Xanomeline alongside trospium
Studies have revealed conflicting outcomes in the exploration of the neurochemical roots of schizophrenia, with dopamine and glutamate, two neurotransmitters, being highlighted as potential contributors to the development of the disorder.
The misuse of amphetamines triggers the release of dopamine and leads to a clinical condition similar to schizophrenia. Antipsychotic medications function by obstructing dopamine receptors in the brain. These foundational concepts paved the way for the dopamine hypothesis. However, the original iteration of this hypothesis has been debunked with the emergence of fresh data. Numerous research ventures have validated that individuals diagnosed with schizophrenia exhibit heightened dopamine synthesis capabilities. To date, only one attempt to replicate these results has proven unsuccessful.
The FDA has recently approved Cobenfy, a novel medication for treating schizophrenia. In a statement, the FDA highlighted that Cobenfy stands out as the initial antipsychotic drug endorsed for addressing schizophrenia by focusing on cholinergic receptors instead of the traditional dopamine receptors, which have been the conventional approach for a long time.
A 2022 review on xanomeline and trospium chloride revealed that the initial development of xanomeline for managing Alzheimer’s disease and schizophrenia was halted due to its negative effects. However, interest in xanomeline resurfaced when researchers contemplated its combined use with trospium. Xanomeline acts as a muscarinic receptor agonist within the parasympathetic nervous system and has the potential to enhance various schizophrenia symptoms. On the other hand, trospium, functioning as an antimuscarinic agent, is anticipated to mitigate the adverse reactions associated with xanomeline.
According to the FDA, Cobenfy is associated with frequent side effects such as nausea, indigestion, high blood pressure, rapid heartbeat, and dizziness. Manufactured by Bristol Myers Squibb, the drug is available at a monthly cost of $1,850.
Support for dealing with suicidal ideation can be accessed through Tele-MANAS 14416, Sneha’s suicide prevention hotline at 044-24640050, and Speak2Us mental health helpline 9375493754.
Alok Kulkarni, a seasoned interventional neuropsychiatrist, practices at the Manas Institute of Mental Health and Neurosciences located in Hubli, Karnataka.