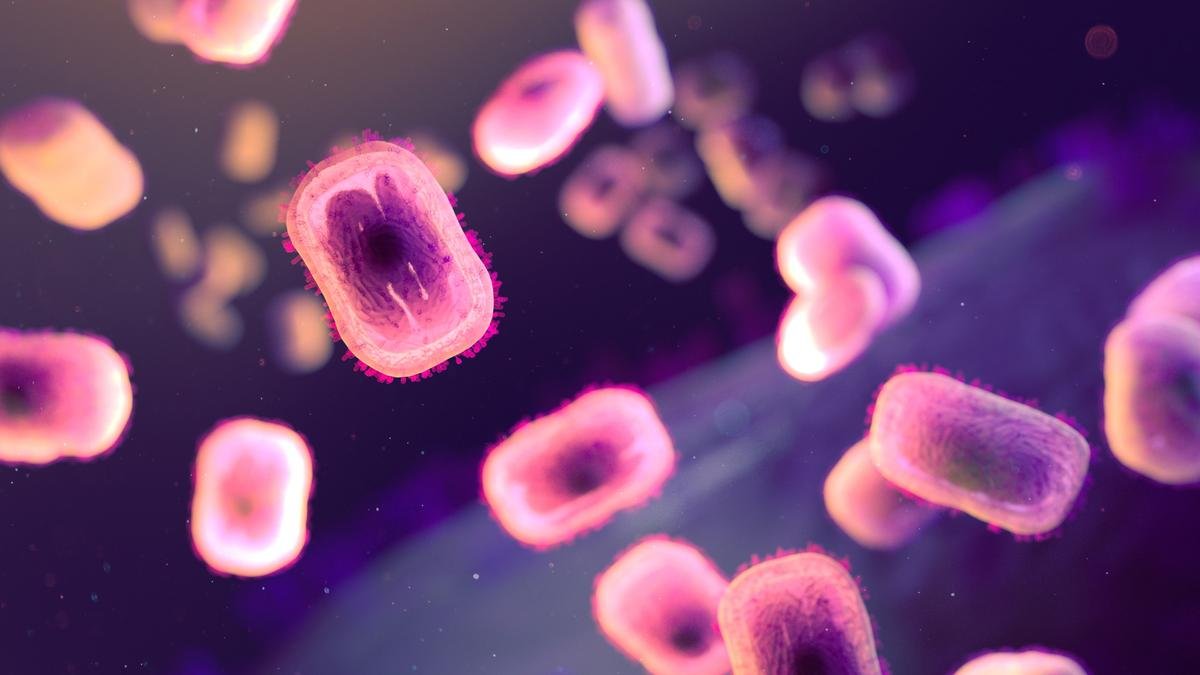
Researchers have found a surge in the prevalence of mutations that can be attributed to a protein family in the human body called APOBEC
Since the world eradicated smallpox in 1980, scientists have known that the battle against poxviruses was far from over. Of the multiple types that exist, scientists have been wary of one in particular: mpox. In fact, one of the points in the World Health Assembly’s post-eradication policies was the “continuation of monkeypox surveillance in West and Central Africa, at least until 1985”.
In August this year, the WHO declared mpox to be a public health emergency for the second time in two years.
(Note: In 2022, the WHO designated “mpox” as a preferred synonym for “monkeypox” disease. The virus is still called “monkeypox” according to the International Committee on the Taxonomy of Viruses. For uniformity’s sake, this article will use “mpox” to refer to both the disease and the virus clades.)
New cause for worry
The declaration ensured multiple countries would pledge vaccines to the 15 African nations affected by the outbreak, six of which had never reported a single case of mpox before. But the paucity of doses has forced countries to prioritise their campaigns. Barely two months since these countries started their targeted vaccinations, scientists have a new cause for worry. A preprint paper uploaded on Virologica, a scientists’ discussion forum online, on October 24 reported evidence that yet another strain of the mpox virus appeared to have achieved human-to-human transmission.
There are two clades of mpox: I and II. Both clades are classified into two subclades, making a total of four known variants: Ia, Ib, IIa, and IIb. Of these, clade IIb was responsible for the 2022 outbreak, which is still continuing in certain parts of Africa.
Clade Ib, discovered towards the end of 2023, is the primary cause of infection in central Africa.
Researchers believed these two clades to be the primary contributors of the present mpox problem. They know very little about clade IIa except that it causes infections in western Africa.
When viruses make ‘mistakes’
It has caused sporadic infections in humans, mostly children, since 1970. However, these infections have always remained confined to a few families or communities, with transmission occurring from animals to humans. There was no evidence of sustained human-to-human transmission — until recently.
The preprint posted on Virologica reported evidence that the DNA of clade Ia viruses sequenced from the present outbreak bears clear signs of human-to-human transmission.
Viruses evolve by introducing changes to their genetic material. Each time a virus infects a new host, an enzyme known as a polymerase makes multiple copies of the virus’s genetic material (DNA or RNA), which is then packed into new viruses. But sometimes the polymerases make a mistake. These mistakes, called mutations, could have a positive, negative or no impact on the virus, meaning the virus can get better or worse or be the same at its job.
The rate at which the polymerases make mutations is different for different viruses. Generally, viruses that have RNA as their genetic material, such as the human immunodeficiency virus (HIV) and influenza, make mistakes much more frequently than those that have DNA, like the human papillomavirus (HPV) and adenoviruses.
This error rate is even lower in some DNA viruses, like the members of the pox family, which also have an error-correction mechanism built into them.
The APOBEC family
However, viral polymerases are not the only source of mistakes in a virus’s genetic material.
The immune system also has a mechanism to introduce random changes in foreign DNA. A family of proteins called APOBEC — short for ‘apolipoprotein B mRNA editing enzyme, catalytic polypeptide-like’ — can introduce changes to the viral DNA while it is being copied in the cells.
APOBEC proteins induce errors in viral DNA, some of which can be lethal to the virus. Notably, of the four DNA bases—adenine, guanine, cytosine, and thymine—viral DNA polymerases can make mistakes at any position. However, APOBEC’s activity typically only alters cytosine to thymine.
In a 2023 study published in Science, researchers demonstrated that APOBEC-induced mutations outnumber those caused by the viral polymerase. They concluded that a sudden surge in mutations in circulating mpox viral DNA must result from APOBEC activity. The researchers argued that since the virus came from human cells, APOBEC likely acted on it, as those mutations would not have appeared so rapidly otherwise.
The researchers also estimated that on average, APOBEC activity would introduce around six mutations every year. Based on how many mutations the researchers observed, and the nature of those mutations, they predicted mpox clade IIb had been circulating in Africa from humans to humans since 2016.
The new study described in the preprint used the same method to show clade Ia viruses have achieved human to human transmission as well.
Viruses’ responses to antivirals
The news that clade Ia viruses can spread from humans to humans is not likely to affect the vaccination strategies of the affected countries. However, it is certainly cause for worry because researchers know that the different mpox clades respond differently to certain antiviral drugs used to treat them.
For now, Africa has pinned its hopes on the few doses of vaccines it has and is hoping against odds that its targeted campaign will suffice to stem the rising tide of mpox cases.
Arun Panchapakesan is an assistant professor at the Y.R. Gaithonde Centre for AIDS Research and Education, Chennai.